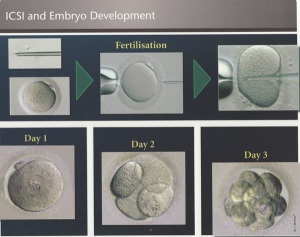
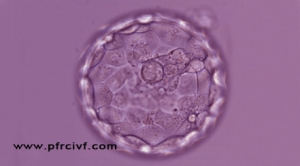
Intra-cytoplasmic sperm injection, commonly referred to as ICSI, is a well-established microinjection technique, which has resulted in additional options for patients in the treatment of their infertility. ICSI involves the insertion of a single selected sperm directly into the cytoplasm of a mature egg, bypassing all the preliminary steps of sperm binding.
This procedure overcomes many barriers to fertilisation which can include failed fertilisation from repeated use of conventional IVF, severe male factor infertility, very low sperm counts and/or motility, high number of morphologically abnormal sperm, utilisation of surgically retrieved sperm, use of frozen sperm when limited in number and quality.
The first human pregnancy with ICSI was reported in 1992 and since this time thousands of babies have been born as a result of the ICSI procedure, providing many couples with hope previously not available.
ICSI enables fertilisation to happen when there are very few sperm available.
Your clinic may recommend ICSI if:
- you have a very low sperm count
- other problems with the sperm have been identified, such as poor morphology (abnormal shape) or poor motility (not moving normally)
- during previous attempts at IVF there was failure of fertilisation or an unexpectedly low fertilisation rate
- you need sperm to be collected surgically from the testicles or epididymis (a narrow tube inside the scrotum, where sperm are stored and matured); for example because you have had a vasectomy, you do not ejaculate sperm, or because you have extremely low sperm production
- you are using frozen sperm in your treatment which is not of optimum quality
- you are using embryo testing.





 Age less than 27
Age less than 27

