The timeline for IVF treatment usually goes something like this:


- Ovary stimulation. For eight to 14 days near the beginning of your menstrual cycle, you take a gonadotropin, a type of fertility drug that stimulates your ovaries to develop multiple mature eggs for fertilization (instead of just one). You also need to take a synthetic hormone like leuprolide or cetrorelix to keep your body from releasing the eggs too early.
- Follicle development. While taking these medications, you visit your doctor's office or clinic every two to three days to have your blood hormone levels checked and ultrasound measurements of your ovaries done. This allows your healthcare provider to monitor development of the follicles – the fluid-filled sacs where eggs mature.
- The trigger shot. When the follicles are ready, you get a "trigger shot," an injection that causes the eggs to mature fully and become capable of being fertilized. About 36 hours after your trigger shot, your eggs are ready to be retrieved.
- Gathering the eggs. Your doctor gives you an anesthetic and inserts anultrasound probe through your vagina to look at your ovaries and identify the follicles. A thin needle is then inserted through the vaginal wall to remove the eggs from the follicles. Eight to 15 eggs are usually retrieved. You may have some cramping and spotting for a few days afterward, but most women feel better in a day or two.
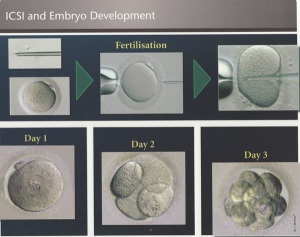
- Fertilization. An embryologist www.pfrcivf.com (a scientist who specializes in eggs, sperm, and embryos) will examine your eggs before combining them with your partner's sperm and incubating them overnight. Fertilization usually happens during this time, but eggs that aren't normal may not be fertilized. (If sperm quality is poor, or if fertilization was unsuccessful during previous IVF cycles, your doctor may recommend using a technique called intracytoplasmic sperm injection (ICSI). With ICSI, a single sperm is injected directly into each mature egg.)
- Developing embryos. Three days after the egg retrieval, some of the eggs that were successfully fertilized become six- to 10-celled embryos. By the fifth day, some of these embryos will become blastocysts with a fluid-filled cavity and tissues that are beginning to separate into placenta and baby.
- Embryo selection. The embryologist selects the most viable embryo or embryos to place in your uterus three to five days after the egg retrieval. Extra embryos, www.pfrcivf.com if there are any, may be frozen and used for future IVF cycles.
- Planting the embryos. Depending on your age and diagnosis, your doctor places between one and five embryos in your uterus by inserting a thin tube (a catheter) through your cervix. You might feel some mild cramping, but you won't need anesthesia.
- Successful implantation. If the treatment works, an embryo implants in your uterine wall and continues to grow into a baby. Keep in mind that if more than one embryo is transferred, your chance of pregnancy is higher, but so are the odds of having a multiple pregnancy – about 20 percent of babies born through IVF aretwins, triplets, or more.