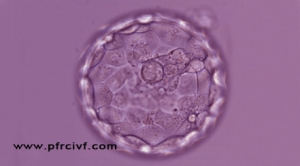
In the past most embryos produced with IVF were transferred on day three of development, known as cleavage stage. When an embryo reaches five days of development it is called a blastocyst. Currently, with advances in understanding of the needs of developing embryos, the ability to produce blastocysts in the laboratory has increased. This extended culture time allows nature to help select those embryos with the highest capacity to produce a pregnancy. Culturing and transferring blastocysts on day five of development allows the transfer of fewer embryos while still maintaining a high pregnancy rate. Normally only two blastocyst stage embryos are transferred, thus reducing the risk of multiple pregnancies higher than twins.
Why Blastocyst Transfer ?
Selection of embryos
We know that at least 50% (or higher in women over 40) of embryos are not viable, and many of these arrest their development before the blastocyst stage. A large proportion of these embryos have a chromosome or genetic defect and it is believed that those embryos that failed to develop to the blastocyst would not, in any event, have established a pregnancy. Where there are large numbers of good quality embryos available at the blastocyst stage these can be frozen. CARE Fertility has seen excellent post thaw survival and pregnancy rates with frozen blastocysts.
Embryos are transferred to the right place at the right time
Some researchers believe that the conditions in the womb may be more optimal for a blastocyst than a day 2/3 embryo as there are slightly differing conditions in the fallopian tube and the womb on day 2/3.
Higher pregnancy rate in women having Blastocyst Transfer
Data suggests that blastocyst transfer can increase the chances of a live birth but it needs to be remembered that each couple must be considered independently.
Confirmation of development to the blastocyst stage
Some specialists believe that for those patients who have recurrent failure of implantation, extended culture gives an opportunity to examine the embryo quality over a longer period. If the embryos arrest or become fragmented this may help to clarify a potential problem.
Specific situations where blastocyst transfer is applicable
Where single embryo transfer is specifically indicated (eg. previous history of multiple pregnancy, patient preference, uterine anomaly etc) blastocyst transfer may be a particularly useful option.
Extended culture and Blastocys Transfer with Frozen Embryos
Some patients have large numbers of frozen embryos and it can difficult to know which have the best potential for pregnancy. An option in these cases is to thaw all embryos and culture through to the blastocyst stage to allow the best 1 or 2 embryos to be replaced based on development.
The main benefit of the blastocyst transfer approach is in the ability to discriminate between different embryos in terms of their quality and implantation potential. It is essential to understand that the extended culture process doesn't enhance an embryos quality per se, it is principally a method for choosing the 'front runner' or 'runners' from a group of embryos.
CARE doctors and embryologists will advise on whether blastocyst transfer is possible this will depend on the number and quality of embryos available on day 3.